Comments on 'Endometriosis is an incredibly interesting disease'
1.5k words, 8 minute reading time
Introduction
My last article over endometriosis is by far the most popular thing I have ever written, with more likes, comments, and views than basically anything else I’ve published over the past year. This is great! But, as with all commentary over human disease that is shorter than a dozen page review paper written in 10-point font, it missed some things. I bathe myself in a river of compassion for this act, and, as an apology, offer a compilation of eight interesting perspectives/corrections given to me by the very patient readers who went through a 5,000 word article:
Comments
Medical imaging is getting better for diagnosis
I mentioned in the article that clinicians currently rely on laparoscopic surgery as the gold standard diagnosis for endometriosis. I have since learned that non-invasive imaging has improved an awful lot in the past few years, and that surgery is often not necessary for a conclusive diagnosis. A private DM and a HN comment alerted me to this. This said, relying on imaging doesn’t seem to have leaked into common practice, given how many other people seemed to bemoan how awful their diagnostic laparoscopic surgery was. From a 2022 review article:
The previous ESHRE guidelines suggested that laparoscopic histologic confirmation of endometriosis was the gold standard for an endometriosis diagnosis. In contrast, according to the new ESHRE guidelines, laparoscopy is no longer the diagnostic gold standard and is now only advised for patients with negative imaging results and/or when empirical treatment is ineffective or unsuitable. This change was based on a meta-analysis regarding endometriosis diagnostic tools. According to a Cochrane review, imaging modalities such as transvaginal ultrasonography and magnetic resonance imaging showed sensitivity and specificity for diagnosing endometrioma and deep endometriosis comparable to a surgical diagnosis
Recurrence rate depends on the type of surgery
I mentioned that post-surgical remission rates are quite high, with the upper-end being 40%~. But there is some nuance to add here. The typical surgical approach to endometriosis is ablative surgery, e.g. burning away the lesions. One HN comment points out that this is a really dumb idea, for the same reason that it is a dumb idea in cancer: the undesirable cells have likely leaked into the surrounding tissue, beyond the visible lesions. An increasing number of surgeons are now electing to do what is done in cancer, which is to excise the lesion directly with healthy margins around the seemingly healthy tissue. A 2021 retrospective study states that doing this vastly reduces recurrence rates compared to ablation. But, as the comment states, most surgeons still perform ablations because that’s what they’ve been taught.
One interesting note is that the story for excision being better isn’t as clear cut for actual symptoms. A 2017 review paper states that excision reduces symptoms compared to ablation, but a 2022 review paper shows no difference at all. More work to be done!
Appearance of endometriosis doesn’t tie well to symptoms
A comment by a clinician on the r/slatestarcodex subreddit notes that appearance of endometriosis doesn’t tie 1:1 to symptom burden. This is something I was aware of and pondered talking about in the article, but decided not to in the end, because it didn’t feel like there was much I could say about it. Lots of conditions have a mismatch between how bad they look and how bad the patient feels, and the best explanation I’ve heard for that is that pain is weird. Comment given here:
Something the article doesn't touch on, but which is equally intriguing is how severity of the lesions seen during laparoscopic surgery DON'T strictly correspond to symptom severity (though they're correlated of course). I remember seeing one surgery, for completely unrelated gallstones, where the inside of a woman's abdomen was incidentally found to be absolutely speckled with black spots... she was asymptomatic. Another woman we found only 2 possible lesions we could biopsy and no adhesions... she had severe pain.
Does pregnancy cure endometriosis?
A few people have commented that pregnancy seems to magically cure endometriosis, including this comment on Substack. This is something I too offhandedly mentioned in the article, but didn’t really follow up on it. But according to one paper that followed 15 women who had endometriosis and achieved pregnancy via IVF, the theory doesn’t seem to be true. Pregnancy does help with endometriosis symptoms initially, but they do return over time. A more recent, comprehensive review paper also supports this. Because of these results, I don’t think there is something very interesting going on, and chalk the ‘regression’ up to the dramatically increased levels of progesterone (which inhibit endometrial cell proliferation and angiogenesis) that come alongside pregnancy. But once those hormone levels disappear, the endometriosis eventually comes back.
Endometriosis is only mildly heritable
One person on LessWrong noted that I was a little fast-and-loose with saying that endometriosis is ‘strongly’ heritable. Quoting from them:
Lastly I have a very minor nitpick. The Nature paper you linked ostensibly showing very high heritability doesn't actually mention heritability in the abstract. The paper made a genetic predictor for endometriosis which explained 5% of the variance (not particularly high, especially given the sample size they were working with).
It does cite a paper about heritability, but that paper doesn't showing endometriosis as being unusually heritable; it shows 47% of the variance can be explained by additive genetic factors. That's pretty middle-of-the-pack as far as heritability goes. Conditions like Alzheimer's and Schizophrenia are significantly more heritable; roughly 70% and 80% respectively.
Actual heritability of Endometriosis is likely somewhat higher than that because most conditions have some non-additive genetic variance. This paper (somewhat questionably) attributes the entire remainder of the variance to "unique environmental factors".
This is helpful context! There is also at least one study in the literature where the heritability rate of the disease was far, far lower than what most others are reporting — only 2x higher chance to get endometriosis, as opposed to 7x-9x higher, if your mom had it. The same LessWrong commenter notes that the disease is ‘shockingly’ polygenic, which maybe helps explain the relative variance people see.
A non-invasive, non-hormonal therapeutic that works as well as surgery
I had one person on Substack mention that there are validated non-hormonal alternatives to endometriosis management. One that they mentioned is ethanol injection — also called sclerotherapy — is particularly interesting since it can preserve fertility in cases where surgery would threaten it and is minimally invasive. But certainly the downside is that it is less effective than surgery, right? Fascinatingly enough, it seems to work roughly as well as excising surgery according to one (albeit small) randomized control trial. Again, it doesn’t seem to have leaked into common practice as of yet.
Do 10% of women actually have endometriosis?
One person on Bluesky mentioned that 10% of reproductive age women (190 million) having endometriosis seems a bit extreme. I’ll admit, I didn’t look into this number too much and took the World Health Organization’s (WHO) number at face value. But where does this value come from? One 2019 survey of 27,000~ reproductive age women in the US came up with 6.4%, and another 2012 study of 62,000~ reproductive age women in Germany came up with a much lower .81%. There’s lots of other studies too, but the general theme is similar: vastly lower numbers than 10%. What’s going on? Did I and the WHO dramatically overestimate the prevalence of the condition?
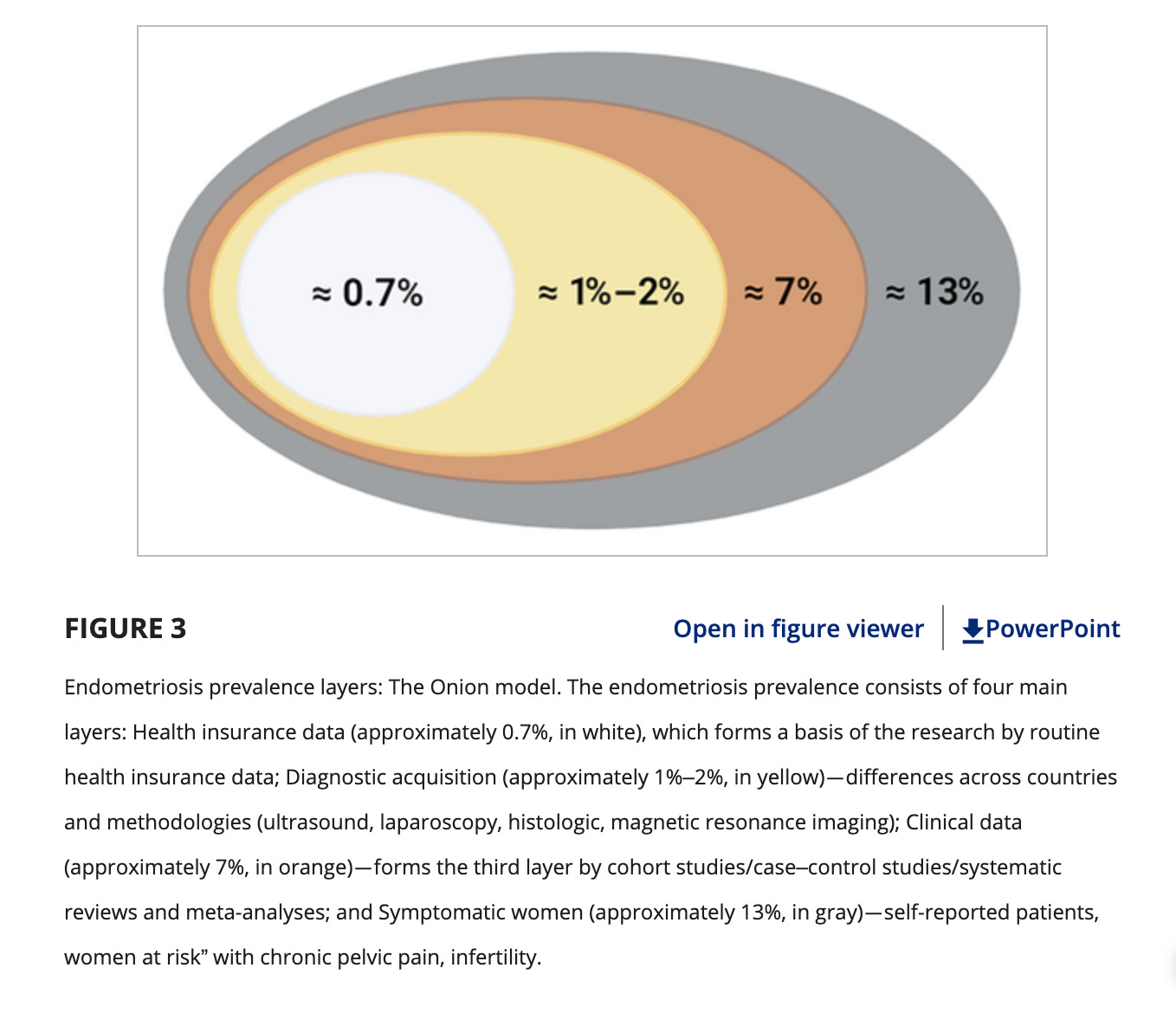
Well, one study examined this strange variance and found that the true population count of the disease depends on what we count as ‘having endometriosis’. On the most strict spectrum, if we consider only ‘having an ICD-10 code for endometriosis’ as evidence for the condition, yes, the true rate is very low, just under 1%. But if we instead consider the likely prevalence of the condition given case studies of certain populations, the number expands to 7%. If we also accept likely endometriosis (the symptoms match or it is self-reported), it balloons to 13%.
To me, 10% feels like a decent short-hand number, but I could also buy that it is mildly inflated. In any case, if we go with 10%, it seems that the whole ‘the disease is under-diagnosed’ pitch is already slightly baked into that number, which reduces the impact of the DALYs:Dollars recalculation I made in the original article. Endometriosis still remains one of the most overlooked diseases, but it perhaps may still be far less overlooked than something like COPD. Here’s a helpful graph:
People are working on better drugs
This isn’t something I could’ve known in advance, but several biotech startup founders read the article and DM’d me to say that they are coincidentally currently doing preclinical work on non-hormonal drugs to aid in endometriosis management. Obviously, that work has years to go to wind itself through the FDA trial process, but still, exciting to hear about!



There is a strong link between genetic predisposition to endometriosis and mental health issues. Women with endometriosis often report feeling unloved, experiencing abuse, or facing trauma at a young age, and they show higher rates of Post Traumatic Stress Disorder (PTSD). This suggests that mental health stressors are one of the factors that can worsen endometriosis in women with specific genetic risk variations. https://www.pillcheck.ca/2025/07/07/understanding-endometriosis-symptoms-risks-and-personalized-treatment/